Resources
Information to aid your rehab journey
Explore our resources to better understand your condition and take charge of your recovery.
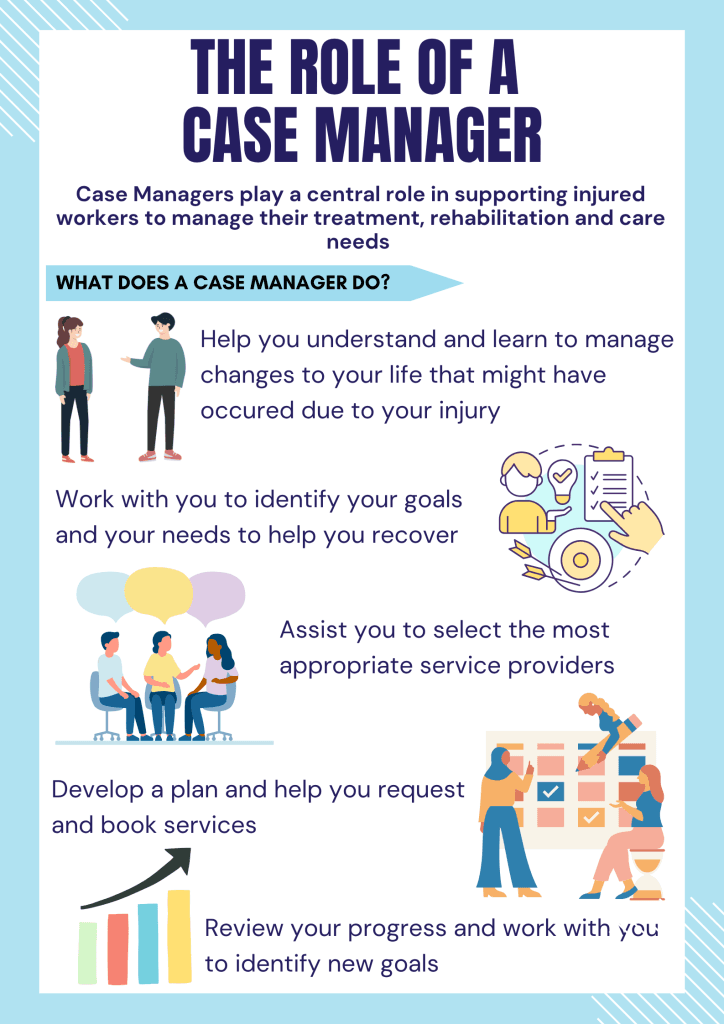
Effective recovery requires a holistic, evidence-based approach that gets results. These resources give you a basic understanding of a range of neurological conditions and physical injuries, offering insights into how expert, multidisciplinary rehabilitation can help you achieve your goals and improve your quality of life.
Post Traumatic Stress Disorder (PTSD)
Post-Traumatic Stress Disorder (PTSD) is a mental health condition caused by experiencing or witnessing traumatic events. It leads to ongoing fear, anxiety, and emotional distress that can affect daily life. Common triggers include accidents, abuse, natural disasters, war, or terrorism.
- Avoidance of reminders
- Loss of interest and social withdrawal
- Difficulty concentrating
- Physical symptoms (e.g. rapid heartbeat, nausea)
- Emotional numbness
- Sleep and mood disturbances
- Flashbacks and nightmares
- Substance use
- Guilt or shame
- Trouble with work or routines
A GP, psychologist, or psychiatrist will:
- Ask about your symptoms and trauma history
- Use screening tools or questionnaires
- Confirm symptoms have lasted over a month and impact daily life
You may be referred to a mental health specialist for further support and treatment.
PTSD can be effectively treated with psychological therapies that help reduce symptoms and support recovery.
Cognitive Therapy for PTSD (CT-PTSD): Helps change negative thoughts and beliefs about the trauma, yourself, and the world. Reduces feelings of ongoing threat and increases sense of safety.
Prolonged Exposure (PE): Involves gradually confronting trauma memories and avoided situations to reduce fear and distress and build healthier coping strategies.
Eye Movement Desensitisation and Reprocessing (EMDR): Uses guided eye movements while recalling traumatic memories to help the brain process and store them, reducing emotional impact.
Cognitive Processing Therapy (CPT): Focuses on identifying and challenging “stuck” thoughts related to trauma. Helps reframe negative beliefs and address emotions like guilt or anger.
Psycho-social Interventions: Emphasises support from family and friends, reducing alcohol or drug use, re-establishing healthy routines, and maintaining a balanced lifestyle with regular exercise.
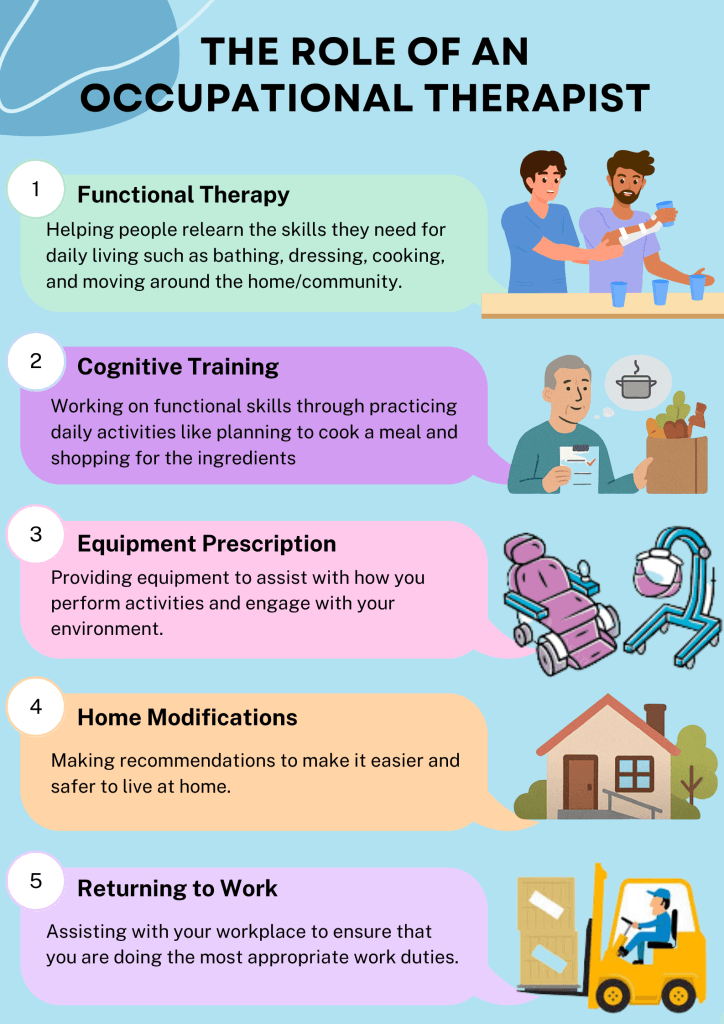
Occupational Therapist: Supports daily functioning by helping individuals manage routines, develop coping strategies, and engage in meaningful activities. Uses trauma-informed approaches to reduce stress and improve independence.
Physiotherapy: Helps manage physical symptoms like muscle tension, pain, or mobility issues that may be linked to trauma. Encourages body awareness and relaxation.
Exercise Physiologist: Designs tailored exercise programs to reduce stress, improve mood, and support physical recovery. Promotes overall wellbeing through movement.
Anxiety
Anxiety is a natural response to stress or danger. It becomes a disorder when it’s persistent, overwhelming, and interferes with daily life.
Anxiety can be an overwhelming and distressing experience, both physically and mentally. Common physical symptoms include:
- racing heart
- shortness of breath
- sweating and/or trembling
- nausea, dizziness and/or restlessness.
Emotionally, it may bring intrusive thoughts, upsetting images, nightmares, and changes in behaviour. These symptoms can interfere with everyday life, relationships, work, and overall wellbeing.
A GP or mental health professional will assess your symptoms, how they affect your life, and may use questionnaires. Diagnosis is based on the severity, duration, and impact of symptoms.
Treatment may include lifestyle changes, medication, and psychological therapies. Common evidence-based therapies include:
Cognitive Behaviour Therapy (CBT): Helps identify and change unhelpful thoughts and behaviours
Dialectical Behaviour Therapy (DBT): Focuses on managing intense emotions and improving relationships
Acceptance and Commitment Therapy (ACT): Encourages acceptance of difficult emotions and commitment to meaningful actions
Eye Movement Desensitisation and Reprocessing (EMDR): Uses guided eye movements to help process trauma and reduce emotional distress
Occupational Therapist: Support emotional regulation, engagement in meaningful activities. They use tools like sensory profiling, behavioural therapy routine planning to reduce social withdrawal and promote independence.
Physiotherapist: Treat physical symptoms of anxiety using breathing techniques, movement therapy, and pacing strategies. They help improve sleep, reduce pain, and support overall wellbeing.
Exercise Physiologist: Designs tailored exercise programs to reduce stress, improve mood, and support physical recovery. Promotes overall wellbeing through movement.
Depression
Depression is a common and serious mental health condition that affects how you feel, think, and function. It goes beyond feeling sad or low – it involves persistent feelings of emptiness, hopelessness, or loss of interest in daily activities.
Emotional & Cognitive:
- Difficulty concentrating
- Persistent sadness or low mood
- Feelings of guilt or worthlessness
- Loss of interest in activities
- Thoughts of self-harm or suicide
- Hopelessness or helplessness
Physical & Behavioural:
- Changes in appetite or weight
- Fatigue or low energy
- Physical symptoms (e.g. headaches, stomach issues)
- Sleep problems (too much or too little)
- Slowed movements or speech
- Withdrawal from social activities
A GP or mental health professional will assess your symptoms, duration, and impact on daily life. Diagnosis typically requires symptoms to last at least two weeks and cause significant distress or impairment. Tools like a questionnaire may be used to support diagnosis.
Medication: Antidepressants may be prescribed, often alongside therapy, especially for moderate to severe depression.
Psychological Therapies:
- Cognitive Behaviour Therapy (CBT): Helps identify and change negative thought patterns and behaviours contributing to depression.
- Dialectical Behaviour Therapy (DBT): Focuses on emotional regulation, distress tolerance, and improving interpersonal skills.
- Acceptance and Commitment Therapy (ACT): Encourages acceptance of difficult emotions and commitment to actions aligned with personal values.
- Eye Movement Desensitisation and Reprocessing (EMDR): Uses guided eye movements to help process trauma-related memories that may contribute to depression.
Occupational Therapist: Help create daily routines, setting achievable goals, and using meaningful activities to improve mood and motivation.
Physiotherapist: Support by relieving physical tension and pain, improving posture and sleep, and using gentle exercises and relaxation techniques to calm the body and mind.
Exercise Physiologist: Use physical activity to boost mental health by releasing feel-good chemicals, improving sleep, and building self-confidence through movement.
Parkinson’s Disease
Parkinson’s disease is a progressive neurological condition that affects movement and coordination. It happens when certain brain cells that produce a chemical called Dopamine start to die. Dopamine helps control smooth and balanced muscle movement, which without enough of it, people may experience tremors, stiffness, and difficulty with movement.
The exact cause of Parkinson’s is still unknown; however, it’s believed to be a mix of genetic and environmental factors such as pesticide or chemical exposure and head injuries. Most cases develop after 50 years of age.
Movement Symptoms:
- Tremors (shaking), especially at rest
- Stiff or rigid muscles
- Slowness of movement (bradykinesia)
- Trouble with balance and walking
- Small, cramped handwriting
Non-Movement Symptoms:
- Depression or anxiety
- Sleep problems
- Constipation
- Low blood pressure when standing
- Memory or thinking changes
- Loss of facial expression
There’s no single test for Parkinson’s. Diagnosis is usually based on:
- A comprehensive neurological exam
- A review of medical history and symptoms
- Brain imaging to rule out other conditions
While there’s no cure yet, many treatments can help manage symptoms and improve quality of life.
Medications: Most people take medicines that boost Dopamine or mimic its effects.
Surgery: Deep Brain Stimulation (DBS) is a surgical option. It involves placing electrodes in the brain to help control movement symptoms.
Occupational Therapist: Helps with daily task management by teaching adaptive techniques for activities such as dressing and showering and teaching energy conservation strategies to reduce fatigue. They can also recommend assistive devices and recommend modifications within the home to make things safer and easier to navigate within the home environment.
Physiotherapist: Improving strength, movement, balance and mobility impairments to improve overall function and reduce the risk of falls. Manual therapy can also assist with reducing muscle stiffness and pain, as well as making it easier to perform safe transfers.
Exercise Physiologist: Assists with creating a safe and tailored home exercise or gym program to incorporate improvements with strength, balance and cardiovascular fitness.
Multiple Sclerosis (MS)
MS is an autoimmune condition where the immune system attacks the brain and spinal cord, damaging myelin – the protective layer around nerves. This disrupts nerve signals and causes scarring (sclerosis). The exact cause is unknown, but genetics, environment, and low Vitamin D may play a role. MS can present in a variety of ways including:
- Relapsing Remitting (RRMS): Most common form. Symptoms flare (relapses) followed by recovery periods (remissions).
- Secondary Progressive (SPMS): Follows RRMS. Relapses lessen, but symptoms steadily worsen.
- Primary Progressive (PPMS): Symptoms gradually worsen from the start, without clear relapses or remissions.
Symptoms of MS can be different from person to person. They can come and go or get worse over time. MS can affect any part of the central nervous system. Symptoms can worsen with heat or during other infections such as urinary tract or respiratory infections. Symptoms can include:
- Depression
- Muscle stiffness
- Difficulty thinking clearly
- Numbness or weakness especially in the arms and legs
- Difficulty walking or keeping balance
- Problems with sexual function or urination
- Fatigue
- Vision problems
A comprehensive Neurological Examination, along with an MRI scan to show scarring on the brain and spinal cord can be used to assist diagnosis. Other tests such as a lumbar puncture and visual evoked potentials can also help support the diagnosis.
Disease-Modifying Therapies (DMTs): DMTs are medications that reduce the frequency and severity of relapses, slow disease progression, and help prevent new damage to the brain and spinal cord. They are available as injections, oral tablets, or infusions.
Occupational Therapist: Assists with daily activities like dressing, cooking, and showering. Recommends assistive devices (e.g. shower chairs, walkers) and teaches energy-conservation strategies to manage fatigue and other impairments.
Physiotherapist: Focuses on improving strength, mobility, balance, and coordination. Helps reduce muscle stiffness, spasms, and pain to support the ability to transfer and move from one place to another.
Exercise Physiologist: Develops tailored exercise programs using aerobic, resistance, and stretching techniques to improve physical function and support individual goals.
Motor Neurone Disease (MND)
Motor Neurone Disease (MND) is a group of progressive neurological conditions that affect the nerve cells (motor neurons) responsible for controlling muscles used for movement, speech, breathing, and swallowing. Over time, these neurons become damaged and die, leading to muscle weakness and wasting. The exact cause of MND is still unknown, but it’s believed to involve a combination of genetic and environmental factors.
Symptoms vary depending on the type of MND and which motor neurons are affected. They usually begin gradually and worsen over time.
Early Symptoms:
- Muscle weakness (often in hands, feet or speech muscles)
- Muscle cramps or twitching
- Slurred speech or difficulty swallowing
- Fatigue and clumsiness
Progressive Symptoms:
- Difficulty walking or using hands
- Breathing problems
- Weight loss and muscle wasting
- Emotional changes (e.g. Laughing or crying unexpectedly)
Diagnosis is based on:
- A comprehensive neurological examination
- Electromyography (EMG) to assess muscle activity
- MRI scans to rule out other conditions
- Blood and genetic tests in some cases
Diagnosis can take time, as symptoms may resemble other conditions.
There is currently no cure for MND, but treatments and therapies can help manage symptoms and improve quality of life.
Medications: Medications such as Riluzole and Edaravone may slow disease progression in some people. Medications can also help manage symptoms like muscle stiffness, saliva control, and mood changes.
Occupational Therapist: Provides support for daily activities to ensure that there remains as much independence as possible. They can also recommend assistive devices and recommend modifications within the home.
Physiotherapist: Focuses on maintaining mobility and reducing muscles stiffness. Ongoing assessments are performed, and mobility recommendations are adapted as symptoms progress and worsen over time.
Exercise Physiologist: Assist with creating a safe exercise program to try and maintain as much muscular strength and cardiovascular fitness as possible.
Huntington’s Disease
Huntington’s disease is a progressive, inherited neurological condition that causes the breakdown of nerve cells in the brain. It affects a person’s ability to move, think, and manage emotions. Over time, it can lead to changes in movement, behaviour, and mental abilities.
Movement Symptoms:
- Involuntary jerking or writhing movements
- Muscle stiffness or rigidity
- Trouble with balance, walking, and coordination
- Difficulty speaking or swallowing
Cognitive Symptoms:
- Trouble with planning, organising, or focusing
- Slowed thinking and difficulty finding words
- Poor judgment and memory problems
Emotional and Behavioural Symptoms:
- Depression, irritability, or mood swings
- Anxiety or obsessive thoughts
- Social withdrawal
- In some cases, psychosis or suicidal thoughts
Diagnosis involves:
- A comprehensive neurological exam to assess movement, reflexes, and mental function
- Neuropsychological testing to evaluate memory, reasoning, and language
- Brain imaging (MRI or CT) to detect changes in brain structure
- Genetic testing to confirm the presence of certain genes
Medications:
- Tetrabenazine and Deutetrabenazine – reduce involuntary movements
- Antidepressants and Antipsychotics – help with mood and behaviour
- Mood stabilisers – manage bipolar symptoms
Occupational Therapist: Assists with daily task management by teaching adaptive techniques for dressing, showering, and conserving energy. Recommends assistive devices and home modifications to improve safety and accessibility.
Physiotherapist: Focuses on maintaining mobility, improving strength and function, and reducing fall risk through balance exercises. Manual therapy may be used to relieve muscle stiffness and improve movement patterns.
Exercise Physiologist: Designs safe, tailored home or gym exercise programs to enhance strength, balance, and cardiovascular fitness.
Spinal Cord Injury (SCI)
A spinal cord injury (SCI) is damage to the spinal cord or the nerves at the end of the spinal canal. The spinal cord is a vital part of the nervous system that carries messages between your brain and the rest of your body. When it’s injured, it can cause permanent changes in movement, sensation, and body functions below the level of the injury.
Can be caused by trauma or non-traumatic conditions:
Traumatic Causes:
- Motor vehicle accidents (most common cause)
- Falls (especially in older adults)
- Sports injuries (e.g. diving into shallow water)
- Acts of violence (e.g. gunshot or stab wounds)
Non-Traumatic Causes:
- Arthritis
- Cancer
- Infections (e.g. abscesses)
- Inflammation or spinal disc degeneration
Symptoms depend on the location and severity of the injury. They may include:
- Loss of movement or paralysis
- Loss of sensation (e.g. touch, temperature)
- Loss of bladder or bowel control
- Difficulty breathing or coughing
- Muscle spasms or exaggerated reflexes
- Pain or stinging sensations
Neurological exams to assess movement and sensation. MRI or CT scans to view the spinal cord and surrounding structures.
Rehabilitation begins once the patient is stable and includes education on self-care and skin care to help manage complications such as pressure injuries.
Occupational Therapist: Help patients re-learn daily tasks and adapt routines to reduce fatigue. Prescribes assistive devices and recommends home modifications for safety and ease.
Physiotherapist: Focuses on regaining muscle activation and strength to improve movement. Provides training in mobility and transfers using various walking aids.
Exercise Physiologist: Supports recovery in later stages by creating exercise routines that improve strength and fitness.
Dementia and Alzheimer’s Disease
Dementia is a general term for a group of symptoms that affect memory, thinking, and social abilities severely enough to interfere with daily life. It’s not a specific disease but rather a syndrome caused by various brain disorders. The most common cause of Dementia is Alzheimer’s disease, which accounts for 60–80% of all cases.
Dementia causes:
- Alzheimer’s disease (Amyloid plaques and tau tangles in the brain, genetic factors and age-related changes)
- Vascular dementia (due to stroke or blood vessel damage)
- Lewy body dementia (abnormal protein deposits)
- Frontotemporal dementia (damage to the brain’s frontal and temporal lobes)
- Mixed dementia (a combination of types)
Alzheimer’s disease is a progressive brain disorder that slowly destroys memory and thinking skills. Over time, it affects a person’s ability to carry out even simple tasks. It is the most common form of Dementia and typically affects people over 65, though younger onset can occur.
Early Symptoms:
- Memory loss (especially recent events)
- Difficulty finding words or following conversations
- Confusion about time or place
- Poor judgment or decision-making
- Mood or personality changes
Later Symptoms:
- Trouble recognising loved ones
- Difficulty walking, swallowing, or speaking
- Needing help with daily tasks
- Hallucinations or delusions
Diagnosis involves:
- Medical history and physical exam
- Cognitive and neurological tests
- Brain imaging (MRI or CT scan)
- Genetic testing in some cases
There is no cure, but treatments can help manage symptoms and improve quality of life.
Medications:
- Cholinesterase inhibitors (e.g. Donepezil) to improve communication between nerve cells
- Memantine to regulate brain activity
Occupational Therapist: Help with daily task management by teaching strategies to promote independence. They can also recommend assistive devices and recommend modifications within the home to make things safer and easier to navigate within the home environment.
Physiotherapist: Focuses on maintaining mobility, improving strength and function and reducing falls risk by implementing balance exercises. Manual therapy can also be utilised to assist with muscle stiffness and improve movement patterns.
Exercise Physiologist: Assist with creating a safe and tailored home exercise or gym program to incorporate improvements with strength, balance and cardiovascular fitness.
Central Cord Syndrome
Central Cord Syndrome (CCS) is the most common type of incomplete spinal cord injury. It occurs when there is damage to the centre of the spinal cord, often in the neck. This damage affects the nerve fibres that carry signals from the brain to the body, especially those controlling the arms and hands.
Common causes include:
- Falls, especially in older adults with arthritis or spinal degeneration
- Hyperextension injuries, where the neck is bent backward suddenly (e.g., in car accidents)
- Herniated discs or bone spurs pressing on the spinal cord
- Spinal stenosis, a narrowing of the spinal canal due to aging
Symptoms can vary depending on the severity of the injury, but typically include:
- Weakness or paralysis in the arms and hands, more than in the legs
- Loss of fine motor control, such as difficulty buttoning a shirt or writing
- Changes in sensation (numbness, tingling, or burning) below the injury
- Bladder dysfunction, including incontinence or retention
- Pain, which may feel like burning or aching in the arms or neck
Diagnosis involves:
- Neurological exams to assess strength, sensation, and reflexes
- MRI or CT scans to view spinal cord compression or damage
- X-rays to check for fractures or alignment issues
There is no single treatment for CCS. Management depends on the cause and severity of the injury.
Occupational Therapist: Incorporates training to re-learn daily tasks and make adaptations to make it easier and less fatiguing on the body. They can also prescribe assistive devices and provide recommendations for home modifications.
Physiotherapist: Focuses on regaining muscle activation and strength to improve movement, along with training mobility and transfers using a variety of different walking aids.
Exercise Physiologist: Utilised in the later stages of recovery to assist with creating exercise routines that can improve strength and fitness.
Aphasia
Aphasia is a condition that affects a person’s ability to communicate. It can impact speaking, understanding, reading, and writing. Aphasia happens when there is damage to the parts of the brain responsible for language.
Common causes include:
- Stroke (most common)
- Traumatic brain injury
- Brain tumors
- Infections or inflammation
- Degenerative diseases
Speaking:
- Trouble finding the right words
- Speaking in short or incomplete sentences
- Using incorrect words or sounds
- Speaking fluently but with nonsense words (Wernicke’s Aphasia)
Understanding:
- Difficulty following conversations
- Trouble understanding spoken or written language
Reading and Writing:
- Difficulty reading aloud or understanding written text
- Trouble writing sentences or spelling correctly
Neurological exams to assess brain function. Imaging tests (MRI or CT scans) to identify brain damage. Language assessments by a Speech Pathologist to evaluate speaking, understanding, reading, and writing.
Speech and Language Therapy is the main treatment for aphasia to assist with restoring language skills and teaching new communication methods.
Functional Neurological Disorder (FND)
Functional Neurological Disorder (FND) is a condition where people experience neurological symptoms such as weakness, movement problems, or seizures that are not caused by structural damage to the brain or nervous system. Instead, the brain has trouble sending and receiving signals properly, even though scans and tests may appear normal.
The exact cause of FND is still being studied, but it is believed to involve a mix of:
- Changes in brain function, not structure
- Disrupted communication between brain regions
- Emotional stress or trauma, though not always present
- Other health conditions, such as chronic pain, fatigue, or mental health issues
Movement:
- Weakness or paralysis (often in one limb or one side of the body)
- Tremors, jerky movements, or abnormal postures
- Difficulty walking or balancing
- Sudden loss of coordination
Dissociative Episodes:
- Episodes that look like epileptic seizures but are not caused by abnormal brain activity
- May involve shaking, collapsing, or unresponsiveness
- Often called functional or dissociative seizures
Sensory and other symptoms:
- Numbness or tingling
- Vision or hearing changes
- Speech difficulties (e.g., slurred speech or inability to speak)
- Cognitive issues like memory or concentration problems
FND is diagnosed by a neurologist based on:
- Detailed history and physical exam
- Positive clinical signs, such as Hoover’s sign (used to test leg weakness)
- Normal test results (e.g., MRI, EEG) that rule out other conditions
- Patterns of symptoms that are typical of FND
FND is treatable, and many people improve with the right care.
Education: Understanding that symptoms are real and reversible can be a powerful first step in recovery.
Occupational Therapist: Incorporates training to re-learn daily tasks and make adaptations to make it easier and less fatiguing on the body using energy conservation strategies.
Physiotherapist: Focuses on movement re-training and motor control exercises, along with gait and balance training.
Exercise Physiologist: Assist with creating exercise routines that can improve strength and fitness and to support long-term physical activity and health.
Complex Regional Pain Syndrome (CRPS)
Complex Regional Pain Syndrome (CRPS) is a chronic pain condition that usually affects one limb (arm, leg, hand, or foot) after an injury, surgery, stroke, or heart attack. The pain is often more severe than expected for the original injury and may be accompanied by changes in skin colour, temperature, swelling, or movement.
The exact cause of CRPS is not fully understood, but it is believed to involve:
- Abnormal responses in the nervous system, including both the peripheral and central nervous systems
- Overactive inflammation and changes in blood flow
CRPS often begins after surgery, fracture, injury or immobilisation such as wearing a splint or cast.
- Severe, burning, or throbbing pain, often out of proportion to the injury
- Increased sensitivity to touch (even light contact can be painful)
- Changes in hair or nail growth
- Changes in skin temperature (hot or cold) and color (red, blue, or pale)
- Stiffness or weakness in the affected limb
- Swelling in the affected area
There is no single test for CRPS. Diagnosis is based on:
- Medical history and physical examination
- Ruling out other conditions
- Observing characteristic signs, such as temperature or color changes, swelling, and pain response
Treatment is most effective when started early and often involves a multidisciplinary approach:
Medications:
- Pain relievers (e.g. NSAIDs, nerve pain medications)
- Corticosteroids to reduce inflammation
- Topical creams or patches
Occupational Therapist: Supports and assists with daily activities to create techniques to manage pain and support better independence. Assistive devices can be prescribed to support daily tasks.
Physiotherapist: Assists with therapy to improve movement and reduce pain with a combination of manual therapy and exercise-based therapy.
Benign Paroxysmal Positional Vertigo (BPPV)
Benign Paroxysmal Positional Vertigo (BPPV) is a common inner ear condition that causes brief episodes of dizziness or a spinning sensation (vertigo). It’s triggered by changes in head position, such as rolling over in bed, looking up, or bending down.
BPPV is caused by tiny calcium crystals (otoconia) in the inner ear becoming dislodged and moving into one of the semicircular canals. These canals help detect head movement and maintain balance. When the crystals move into the wrong part of the inner ear, they interfere with normal fluid movement, sending false signals to the brain and causing vertigo.
Common triggers or risk factors include:
- Head injury
- Aging (more common in people over 50)
- Inner ear infections
- Prolonged bed rest or inactivity
Symptoms of BPPV are usually brief but intense and may include:
- A spinning sensation (vertigo) lasting seconds to a minute
- Dizziness when changing head position
- Nausea or vomiting
- Loss of balance or unsteadiness
- Lightheadedness
BPPV is diagnosed through a physical exam and specific head movement tests. A common test is the Dix-Hallpike maneuver, where your doctor or therapist moves your head and body into certain positions while watching your eye movements.
The most effective treatment for BPPV is a series of head and body movements designed to move the dislodged crystals back to their proper place called the Epley Manoeuvre.
Traumatic Brain Injury (TBI)
A Traumatic Brain Injury (TBI) is a disruption in normal brain function caused by a blow, jolt, or penetrating injury to the head or body. TBIs can range from mild (like a concussion) to severe, potentially leading to long-term disability or even death.
TBI can result from:
- Assaults or violence
- Motor vehicle accidents
- Blast injuries (common in military settings)
- Penetrating injuries (e.g. gunshot wounds)
- Falls (especially in older adults and young children)
- Sports injuries
Physical:
- Headache
- Nausea or vomiting
- Dizziness or balance problems
- Fatigue or drowsiness
- Seizures
- Loss of consciousness
Cognitive and Emotional:
- Confusion or disorientation
- Memory or concentration problems
- Mood swings, irritability, or depression
- Sleep disturbances
Sensory:
- Blurred vision
- Ringing in the ears
- Sensitivity to light or sound
- Changes in taste or smell
Diagnosis may include:
- Neurological exams to assess reflexes, coordination, and mental status
- Imaging tests like CT scans or MRIs to detect bleeding, swelling, or fractures
Treatment depends on the severity of the injury and the associated symptoms as each individual can have differing presentations.
Occupational Therapist: Incorporates training to re-learn daily tasks and make adaptations to make it easier and less fatiguing on the body. They can also prescribe assistive devices and provide recommendations for home modifications.
Physiotherapist: Focuses on regaining muscle activation and strength to improve movement, coordination and balance training, along with mobility and transfer training using a variety of different aids.
Exercise Physiologist: Utilised in the later stages of recovery to assist with creating exercise routines that can improve strength and fitness.
Acquired Brain Injury (ABI)
An Acquired Brain Injury (ABI) refers to any damage to the brain that occurs after birth and is not related to a congenital or degenerative condition. ABI can affect a person’s physical, cognitive, emotional, and behavioural functioning, and may be temporary or permanent.
ABI can result from a wide range of causes, including:
- Brain tumours
- Lack of oxygen to the brain (e.g. near-drowning, cardiac arrest)
- Degenerative neurological conditions (e.g. Parkinson’s disease, Alzheimer’s disease)
- Stroke
- Infections (e.g. meningitis, encephalitis)
- Substance abuse (e.g. alcohol or drug-related brain damage)
- Traumatic brain injury (TBI) – from falls, car accidents, sports injuries, or assaults
Physical:
- Weakness or paralysis
- Poor balance or coordination
- Fatigue or sleep disturbances
- Seizures
- Headaches
Cognitive:
- Changes in vision, smell, or touch
- Memory problems
- Difficulty concentrating or paying attention
- Trouble with planning, organising, or decision-making
- Confusion or slowed thinking
- Communication difficulties (e.g., word-finding, following conversations)
Sensory:
- Mood swings or irritability
- Anxiety or depression
- Personality changes
- Impulsivity or poor judgment
Diagnosis may include:
- Brain imaging (e.g. CT or MRI scans) to assess structural damage
- Neuropsychological testing to evaluate memory, attention, and problem-solving
- Functional assessments to understand how the injury affects daily life
Treatment depends on the cause and severity of the injury and often involves a multidisciplinary rehabilitation team.
Medical Treatment:
- Managing the underlying cause (e.g. stroke, infection)
- Medications for symptoms like seizures, mood changes, or pain
Occupational Therapist: Incorporates training to re-learn daily tasks and make adaptations to make it easier and less fatiguing on the body. They can also prescribe assistive devices and provide recommendations for home modifications.
Physiotherapist: Focuses on regaining muscle activation and strength to improve movement, coordination and balance training, along with mobility and transfer training using a variety of different aids.
Exercise Physiologist: Utilised in the later stages of recovery to assist with creating exercise routines that can improve strength and fitness.
Amputation
Amputation refers to the removal of a limb or part of a limb due to injury, disease, or surgical necessity. It can be either traumatic (e.g. from an accident) or surgical (e.g. due to complications from diabetes, cancer, or infection).
Amputation may result from a variety of causes, including:
- Cancer – bone or soft tissue tumors requiring surgical removal
- Peripheral vascular disease – often related to diabetes or atherosclerosis
- Congenital conditions – limb deficiencies present at birth
- Trauma – motor vehicle accidents, workplace injuries, or combat-related injuries
- Infection – severe infections that do not respond to treatment
- Pain at the site of amputation or in the residual limb
- Muscle weakness or joint stiffness
- Phantom limb sensations or pain
- Skin breakdown or pressure sores
- Swelling or sensitivity in the residual limb
- Fatigue due to increased energy demands
- Difficulty with mobility and balance
Diagnosis and assessment typically involve:
- Medical imaging – to evaluate tissue damage or vascular supply
- Functional assessments – to determine mobility, strength, and independence
- Psychological evaluation – to assess emotional adjustment and coping
- Prosthetic assessment – to determine suitability and fit for a prosthesis
Treatment is multidisciplinary and focuses on physical recovery, emotional adjustment, and functional independence.
Medical Treatment:
- Wound care and infection management
- Pain management (including phantom limb pain)
Occupational Therapist: Incorporates training to re-learn daily tasks and make adaptations to make it easier and less fatiguing on the body using energy conservation strategies. They can also prescribe assistive devices and provide recommendations for home modifications.
Physiotherapist: Focuses on strengthening and conditioning the limbs, balance and gait training, mobility and transfer training using aids or prosthetics, along with scar management and desensitisation training.
Exercise Physiologist: Assist with creating exercise routines that can improve strength and fitness and support long-term physical activity and health.
Peripheral Nerve Damage
Peripheral nerve damage, also known as peripheral neuropathy, refers to injury or dysfunction of the nerves outside the brain and spinal cord. These nerves control sensory, motor, and autonomic functions. Damage can lead to pain, weakness, numbness, and coordination issues, often starting in the hands or feet.
Peripheral nerve damage can result from a wide range of causes, including:
- Diabetes mellitus – the most common cause
- Alcohol abuse
- Chemotherapy – drug-induced nerve toxicity
- Vitamin deficiencies – especially B12
- Infections – e.g. Shingles, Lyme disease, HIV
- Trauma or repetitive stress – e.g. carpal tunnel syndrome
- Autoimmune diseases – e.g. Lupus, Guillain-Barré syndrome
Motor:
- Muscle weakness or twitching
- Difficulty walking or balancing
- Muscle atrophy over time
Sensory:
- Numbness or reduced sensation
- Tingling or “pins and needles”
- Burning or sharp pain (often worse at night)
- Hypersensitivity to touch
Diagnosis typically involves:
- Neurological examination – reflexes, strength, sensation
- Nerve conduction studies and Electromyography (EMG)
- Blood tests – to identify metabolic or autoimmune causes
- Imaging (MRI/CT) – to rule out nerve compression
Treatment focuses on managing the underlying cause, relieving symptoms, and improving function.
Medical Treatment:
- Medications – Gabapentin, Duloxetine, Pregabalin for nerve pain
- Topical treatments – Lidocaine patches or creams
- Antidepressants – for pain modulation
- Surgical intervention – if nerve compression is present
Occupational Therapist: Incorporates training to re-learn daily tasks and make adaptations to make it easier and less fatiguing on the body using energy conservation strategies. Training for sensory re-education and fine motor coordination skills can also be implemented.
Physiotherapist: Focuses on strengthening and conditioning exercises along with nerve gliding and desensitisation techniques. Training for the use of assistive devices, along with balance and gait training can be implemented to improve mobility and safety.
Exercise Physiologist: Assist with creating exercise routines that can improve strength and fitness and support long-term physical activity and health.
Polytrauma
Polytrauma refers to multiple traumatic injuries occurring simultaneously in different body regions or organ systems. These injuries are often life-threatening and require complex, co-ordinated medical and rehabilitative care. Unlike isolated trauma, polytrauma overwhelms the body’s ability to cope, triggering systemic responses that can affect even uninjured organs.
Polytrauma typically results from high-energy impacts or catastrophic events, such as:
- Motor vehicle accidents
- Falls from significant heights
- Industrial or workplace accidents
- Violence or penetrating injuries
Physical:
- Head trauma or traumatic brain injury (TBI)
- Chest injuries (e.g. rib fractures, lung contusions)
- Abdominal injuries
- Orthopaedic fractures
- Burns and wounds
- Amputations
Functional Impairments:
- Mobility limitations
- Pain and fatigue
- Sensory deficits (vision, hearing)
- Swallowing or speech difficulties
Psychological and Cognitive Effects:
- Post-traumatic stress disorder (PTSD)
- Anxiety or depression
- Cognitive impairments (e.g., memory, attention)
- Emotional distress or adjustment difficulties
Diagnosis involves a multidisciplinary trauma assessment, including:
- Injury Severity Score (ISS) – a score of 16+ typically indicates polytrauma
- Abbreviated Injury Scale (AIS) – injuries rated 3+ in two or more body regions
- Imaging (CT, MRI, X-rays)
- Laboratory tests – to monitor organ function and inflammation
Treatment is time-sensitive and multidisciplinary, beginning with acute stabilisation and followed by long-term rehabilitation.
Occupational Therapist: Incorporates training to re-learn daily tasks and make adaptations to make it easier and less fatiguing on the body using energy conservation strategies. Modifications to the home environment can also be implemented, along with the prescription of assistive devices.
Physiotherapist: Focuses on strengthening and conditioning exercises along with pain management and desensitisation techniques. Training for the use of assistive devices, along with balance and gait training can be implemented to improve mobility and safety.
Exercise Physiologist: Assist with creating exercise routines that can improve strength and fitness and support long-term physical activity and health.
Vision Loss
Vision loss refers to a partial or complete reduction in visual function, which may affect one or both eyes. It can range from mild visual impairment to total blindness. One specific type of vision loss is Hemianopia, which involves the loss of half of the visual field in one or both eyes, typically caused by damage to the brain rather than the eyes themselves.
Vision loss can result from a wide range of causes, including:
- Traumatic brain injury
- Stroke
- Multiple Sclerosis
- Brain tumors or lesions
- Alzheimer’s disease or other neurodegenerative conditions
- Infections affecting the brain (e.g. Meningitis, Encephalitis)
- Homonymous Hemianopia: Same side vision loss in both eyes
- Heteronymous Hemianopia: Opposite sides affected in each eye (Bitemporal: outer halves lost; Binasal: inner halves lost)
- Superior/Inferior Hemianopia: Top or bottom halves of vision lost
- Quadrantanopia: Loss of a quarter of the visual field
- Loss of vision on one side (left or right) or in specific quadrants
- Visual hallucinations (e.g. flashes or shapes)
- Blurred or double vision
- Loss of depth perception
- Difficulty seeing in low light or at night
- Difficulty reading or navigating crowded environments
Diagnosis involves:
- Visual field testing
- Eye examination
- Neuroimaging (CT/MRI) – to identify brain lesions or stroke
- Neurological assessment – to evaluate associated cognitive or motor deficits
Treatment focuses on managing the underlying cause and adapting to vision changes. Recovery may be partial or permanent depending on the severity.
Occupational Therapist: Incorporates training to re-learn daily tasks and make adaptations with visual compensation strategies, along with environmental modifications to reduce hazards.
Physiotherapist: Focuses on balance and mobility training, especially for safe navigation within the home and community environments. Spatial awareness exercises can also be prescribed.